Perspective - (2022) Volume 11, Issue 2
ADVERSE DRUG REACTIONS ON THE EFFECTIVENESS OF TUBERCULOSIS TREATMENT
Henrick Dudley*Received: May 27, 2022, Manuscript No. JHRP-22-69505; Editor assigned: May 30, 2022, Pre QC No. JHRP-22-69505 (PQ); Reviewed: Jun 13, 2022, QC No. JHRP-22-69505; Revised: Jun 20, 2022, Manuscript No. JHRP-22-69505 (R); Published: Jun 30, 2022, DOI: 10.30876/2321-0958.22.11.183
Description
Anti-Tuberculosis Therapy (ATT) is widely accessible and has an effectiveness rate of more than 90%. The difficulties in attaining this objective, however, continue since ATT can result in Adverse Drug Reactions (ADR) that raise morbidity and undermine adherence, ultimately causing treatment failure, relapse, or the establishment of resistant strains. The World Health Organization (WHO)-recommended ATT is a Fixed-Dose (FDC), single-tablet combination of four drugs (rifampicin, isoniazid, pyrazinamide, and ethambutol) during the intensive phase of treatment, followed by rifampicin and isoniazid in FDC until the end of treatment. This recommendation has been in effect in Brazil since 2009. In Brazil, retrospective investigations indicated that the incidence of ADR ranged from 23 to 83 percent, and in a meta-analysis that also included research from other countries, the incidence ranged from 8.4 to 83.5 percent. ADRs are complex, with the patient’s age, nutritional state, use of alcohol, liver and kidney function, and HIV infection serving as the main determinants.
Antiretroviral Therapy (ART) and ATT co-administration increases the risk of medication interactions, immunopathological reactions, and Adverse Drug Reactions (ADRs) in HIV-Positive Individuals (PLHIV). After six months of ATT, ADRs have been linked to an almost twofold increased risk of unsuccessful treatment results. Adverse drug reactions (ADR) present a hazard to effective anti-tuberculosis therapy. This study set out to assess how treatment outcomes were impacted by ATT-associated ADR and associated variables. A prospective cohort research was conducted from 2010 to 2016 on patients with tuberculosis at a referral facility in Rio de Janeiro, Brazil. ADRs were prospectively recorded, along with good (cure and completion of therapy) and unfavourable (death, loss to follow-up, and failure) outcomes. To calculate the probability of ADR-free period, the Kaplan-Meier curve was utilised. In order to specify independent connections with negative outcomes, a logistic regression model was used. There were 550 individuals enrolled, and 35.1% of them had HIV (PLHIV). ADR took place in 78.6% of individuals and was linked to successful outcomes. Smokers and drug users showed a higher likelihood of adverse results. Grade 3/4-ADR, particularly “liver and biliary system problems,” was more common in PLHIV.
Hepatotoxicity was linked to lower CD4 levels (p=0.03). Male sex, a lack of education, smoking, illegal drug use, alcoholism, and prior ART in PLHIV are all independent risk factors for poor outcomes. Although ADR is more severe in PLHIV and associated with a higher risk of hepatotoxicity, it enhances the likelihood of positive outcomes. Signs and symptoms (clinical), abnormal lab test results (laboratory), or both were used to identify ADR (clinical and laboratory). The WHO-ART classification was used to classify ADRs. The Division of AIDS table for classifying the severity of adult and pediatric ADR formed the basis for the intensity scale: Grade 1: mild event, Grade 2: moderate event, Grade 3: severe event, Grade 4: potentially life-threatening incident, Grade 5: death. Using the Naranjo Scale, the causality of ADRs was classified as being implausible, possible, probable, or unquestionably related to the drugs. Only ADR that was most likely, possibly, or definitely connected was taken into account. The results of ineffective ATT may negatively affect TB control methods directly. Our study’s main conclusions were that ADR was not associated with unfavourable outcomes and that PLHIV participants had higher levels of ADR intensity than HIV- unexposed study participants. These higher levels of ADR intensity were primarily associated with liver and biliary system disorders, particularly in those with lower CD4 counts. In conclusion, poor outcomes during ATT were independently correlated with male sex, low education, smoking habit, and illegal drug use. Alcohol usage and prior ART use were risk factors for adverse outcomes in PLHIV. ADR was more common early on in TB treatment, although it was not linked to bad outcomes.

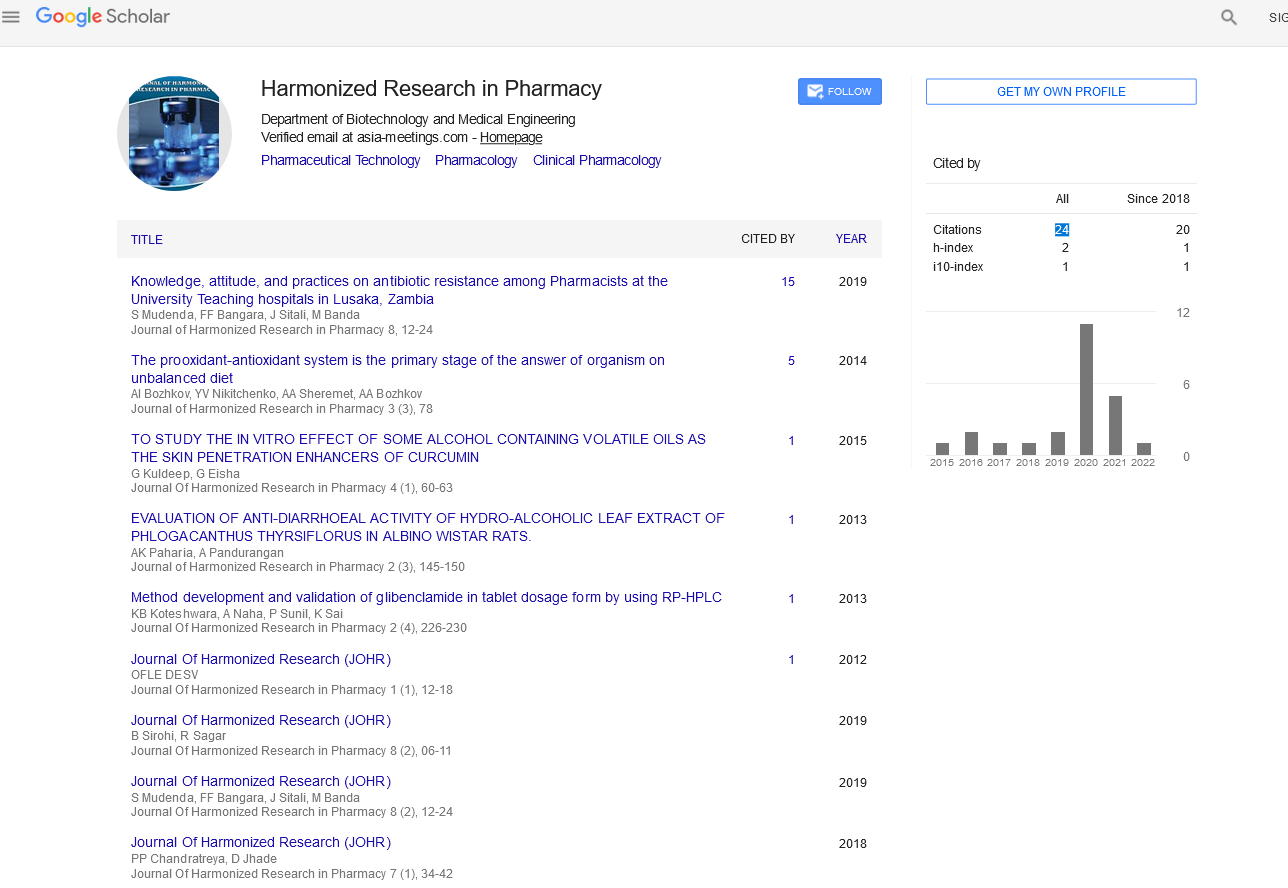
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report