Commentary - (2022) Volume 11, Issue 3
CLINICALLY BENEFICIAL HOSPITAL ADMISSIONS PREDICTION IN THE OLDER POPULATION
Sivapalan Javier*Received: Sep 01, 2022, Manuscript No. JHRP-22-77706 ; Editor assigned: Sep 05, 2022, Pre QC No. JHRP-22-77706 (PQ); Reviewed: Sep 19, 2022, QC No. JHRP-22-77706 ; Revised: Sep 27, 2022, Manuscript No. JHRP-22-77706 (R); Published: Oct 05, 2022, DOI: 10.30876/2321-0958.22.11.189
Description
Older age is typically connected with greater health-related needs and increased healthcare costs, but not by as much as originally anticipated due to an increase in the ageing population around the world. However, there are differences in the correlation between healthcare consumption and prices, and in some highincome nations, healthcare spending per person actually declines dramatically after age 75. The handling of elderly patients who are frail, differences in provider systems, and cultural norms, particularly those that apply close to the moment of death, may all have an impact on how strongly the healthcare system itself affects the relationship between age and healthcare expenditures.
Even though the challenges that an ageing population will pose to the healthcare system may have been overstated, the current state of healthcare for the aged population in many nations is inadequate and not tailored to meet their needs. Morbidity, multimorbidity, and frailty are all factors in the healthcare of the ageing population. However, a number of statistics also show that the majority of the elderly population is content with their health, manages life at home, and believes they are healthy. Only a small percentage of elderly people require hospital care. Most of the time, the healthcare system arranges both hospital and primary care using a passive and reactive (acting when symptoms or issues occur) strategy, failing to distinguish the diverse old-age population.
There have been numerous attempts to classify “frail” older persons in order to identify those who require extensive care (hospital care). But in this situation, the scales that are used to predict people who need medical attention-some of whom are frail-shows some serious flaws. First off, there is no universally agreed-upon operational definition for the medical condition known as “frailty.” Second, and more crucially from a clinical standpoint, clinical instrument evaluation requires trained personnel for each individual examination and is not always straightforward to apply in a larger clinical environment where a primary geriatric perspective might not always be available (primary care, acute ward disciplines).
More recently, the use of computerised administrative data to pinpoint older persons living in communities who are at a high risk for hospitalisation showed good accuracy. We wanted to see if we could create a digital prediction model for older adults who are at high risk for hospital care that could be used in everyday healthcare in the current study, which is why we looked into a larger county population without being restricted by health insurance systems or other selection factors. If this old population could be located, pre-emptive healthcare measures may be taken before receiving hospital treatment.
The fact that most old persons (75% of those aged 80 and beyond) appear to manage themselves at home, despite multi-morbidity and frailty, represents a final constraint of the use of “frailty” measures in a broader clinical setting. This was shown in two distinct studies on 85-year-olds (England, Sweden), which came to identical conclusions about ageing and health. The majority (>75%) of the 85-year-olds in the study handled their lives at home, thought of themselves as healthy (80% gave that rating), and rarely needed hospital treatment. These details highlight how challenging it is to provide healthcare in an elderly population. Prior to hospitalisation, we are not very good at identifying people who might need help and allocating care resources to those who really need it.
The healthcare provider can allocate proactive resources toward a group in greater need thanks to the prediction of the target population for these examinations and interventions, potentially increasing the capacity and cost-effectiveness of the interventions. We offer a therapeutically relevant prediction model for hospital admissions of elderly, potentially vulnerable patients with acceptable accuracy. We explain how it can be applied in a clinical primary care setting and how healthcare organisations might concentrate their resources on clinically pertinent subpopulations.

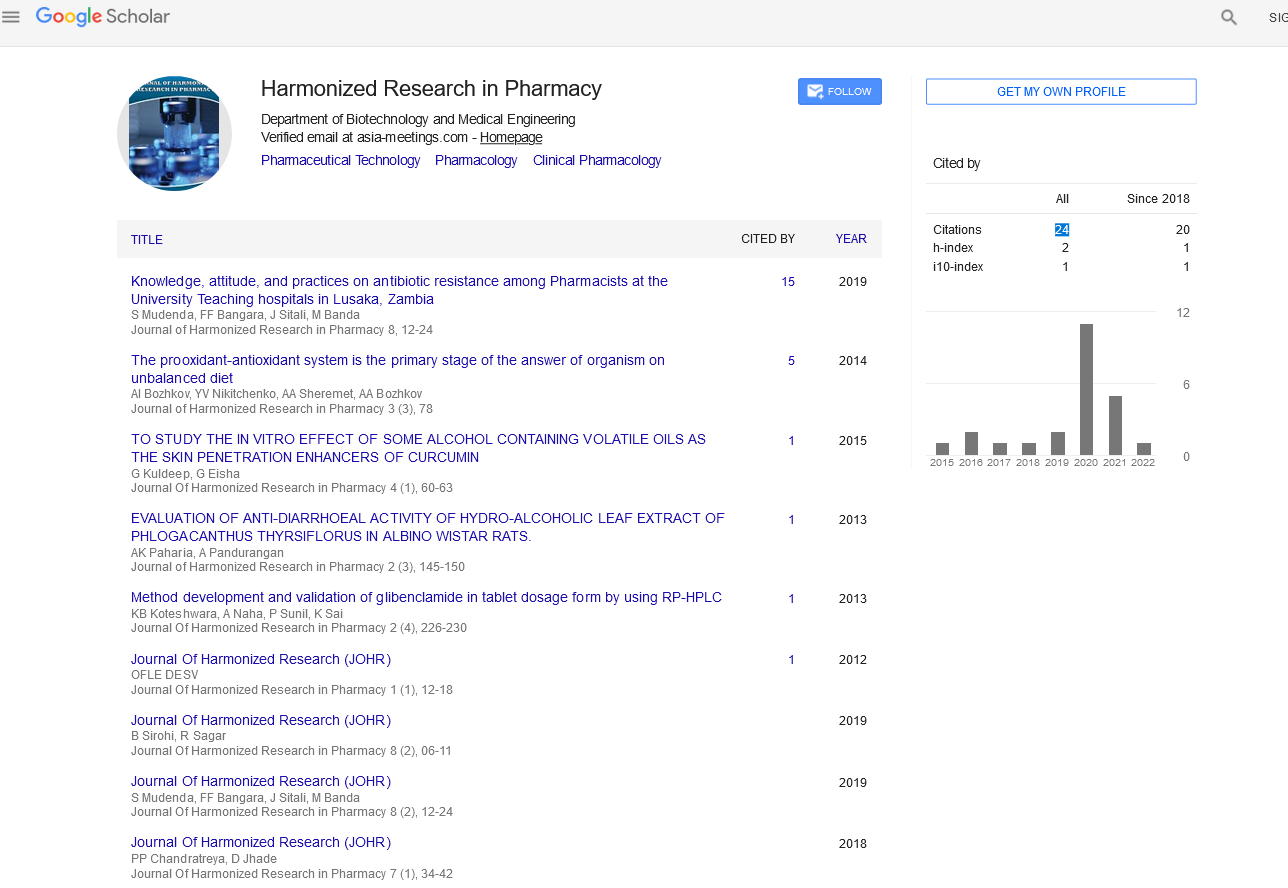
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report