Opinion Article - (2022) Volume 10, Issue 3
ENGINEERING BIOCOMPATIBLE HYDROGEL FIBERS FOR NEURAL TISSUE ENGINEERING WITH VARIABLE MECHANICAL PROPERTIES
Rodrigues Ahmad*Received: Sep 01, 2022, Manuscript No. JHRE-22-77551 ; Editor assigned: Sep 05, 2022, Pre QC No. JHRE-22-77551 (PQ); Reviewed: Sep 19, 2022, QC No. JHRE-22-77551 ; Revised: Sep 27, 2022, Manuscript No. JHRE-22-77551 (R); Published: Oct 05, 2022, DOI: 10.30876/2347-7393.22.10.204.
Description
In order to restore the lost or damaged neurons and axonal pathways that come along with disorders like Traumatic Brain Injury (TBI), stroke, spinal cord injury, and neurodegenerative diseases, the Central Nervous System (CNS) has a limited capacity to generate new cells. The number of people with disabilities (276 million in 2016) and fatalities (9 million in 2016) due to neurological illnesses, which include stroke, dementia, meningitis, and others, is on the rise every year. Although neurogenesis is a multi-step process of neural stem cell development in the CNS, it is only possible in a few number of regions of the brain (such as the hippocampus and dentate gyrus), which makes it difficult to replace lost neurons [1].
Additionally, the absence of directed guidance and inhibitors like glial scar or myelin render regeneration of damaged axonal routes in the CNS ineffective. Due to low cell engraftment and insufficient growth factor localization, conventional regenerative approaches to treat neurological illnesses, such as gene therapy, stem cell transplantation/engraftment, or growth factor delivery, have had only modest success in producing functioning tissues. Animal models are frequently used in regenerative medicine research and CNS problem treatments as a more conventional approach. However, in addition to the exorbitant expenses and associated ethical considerations, the discrepancies between animal models and the human body have raised fundamental doubts about the applicability of animal models. Numerous steps have been taken to establish trustworthy solutions for these important concerns, and in vitro disease models [2].
To create 2D cell-laden constructions, a variety of in vitro techniques have been used, including soft lithography, laser texturing, electrospinning, and electrospraying. These methods, however, fall short of perfectly simulating the mechanical characteristics, architectural design, and physiological makeup of the brain’s unique structure and function. In fact, 2D culture techniques totally or only partially restore the functions of brain cells (including morphology, proliferation, and differentiation). Three- dimensional (3D) bioprinted structures have shown unprecedented potential in simulating the functional native-like tissue microenvironment, in contrast to the 2D techniques. Cells, biomaterial, and bioactive compounds can be precisely positioned in 3D bioprinting to replicate in vivo circumstances. Future progress in developing a quick, affordable, and anatomically correct depiction to solve the current problems with CNS disorders is greatly enhanced by these therapies [3].
In order to create a 3D scaffold that meets the cell proliferation requirements, a typical method is to use aligned polymer nanofibers. The electrospun nanofibers can replicate the original neuroanatomical architecture by regulated neurite outgrowth and cell alignment. For instance, a 3D scaffold made of Bacterial Nanocellulose (BNC) can demonstrate that it can provide brain cells with a biocompatible environment (neuroblastoma, SH-SY5Y). Additionally, the nanofibers and carbon nanotubes can be combined to form a conductive threedimensional composite scaffold that enables extraordinary cell (SH-SY5Y) adhesion and proliferation in accordance with predetermined patterns. For directing cell spreading and proliferation, in addition to nanofibers, other techniques like chemical surface treatment, mechanical stimulation, and surface patterning can be used. Although these techniques can offer a platform for guiding cells that is generally acceptable, their complexity in simultaneously manipulating many cell types and their greater manufacturing costs remain major obstacles [4,5].
Conclusion
A fibre made of a cell-filled composite hydrogel with adjustable mechanical characteristics was created. Core-shell fibres with a cell-laden core and shell were created using a microfluidic device from a biocompatible GelMA/gelatin hybrid hydrogel. The focus of this study was on the quantification of the cellular alignment and tunability of the scaffold structures specifically for brain cells, despite the fact that there have been many prior studies on the application of coaxial bioprinting. Within the fiber’s central axis, the hydrogel fibres displayed cell adhesion, proliferation, and good growth. The fibres produced a well aligned cell arrangement and directed axonal outgrowth.
References
- Ilardo ML, Speciale A. The community pharmacist: perceived barriers and patient-centered care communication. Int J Environ Res Public Health. 2020;17(2):536.
- Shimada H, Ikuta H, Kumazawa K, Nomi M, Shiojiri M, Kawase A, et al. Relationship between the risk of idiosyncratic drug toxicity and formation and degradation profiles of acyl-glucuronide metabolites of nonsteroidal anti-inflammatory drugs in rat liver microsomes. Eur J Pharm Sci. 2022;106193.
[Crossref] [Google Scholar] [Pubmed]
- Al Badi K. Discrete event simulation and pharmacy process re-engineering. Int J Health Care Qual Assur. 2019;32(2):398-411.
[Crossref] [Google Scholar] [Pubmed]
- Gupta R, Rajpoot K, Tekade M, Sharma MC, Safavi M, Tekade RK. Factors influencing drug toxicity. Pharmacok. 2022; 27-50.
- Sengupta P, Chatterjee B, Tekade RK. Drug toxicity and forensic pharmacokinetics. Pharmacok Toxicok Consid. 2022; 425-486.

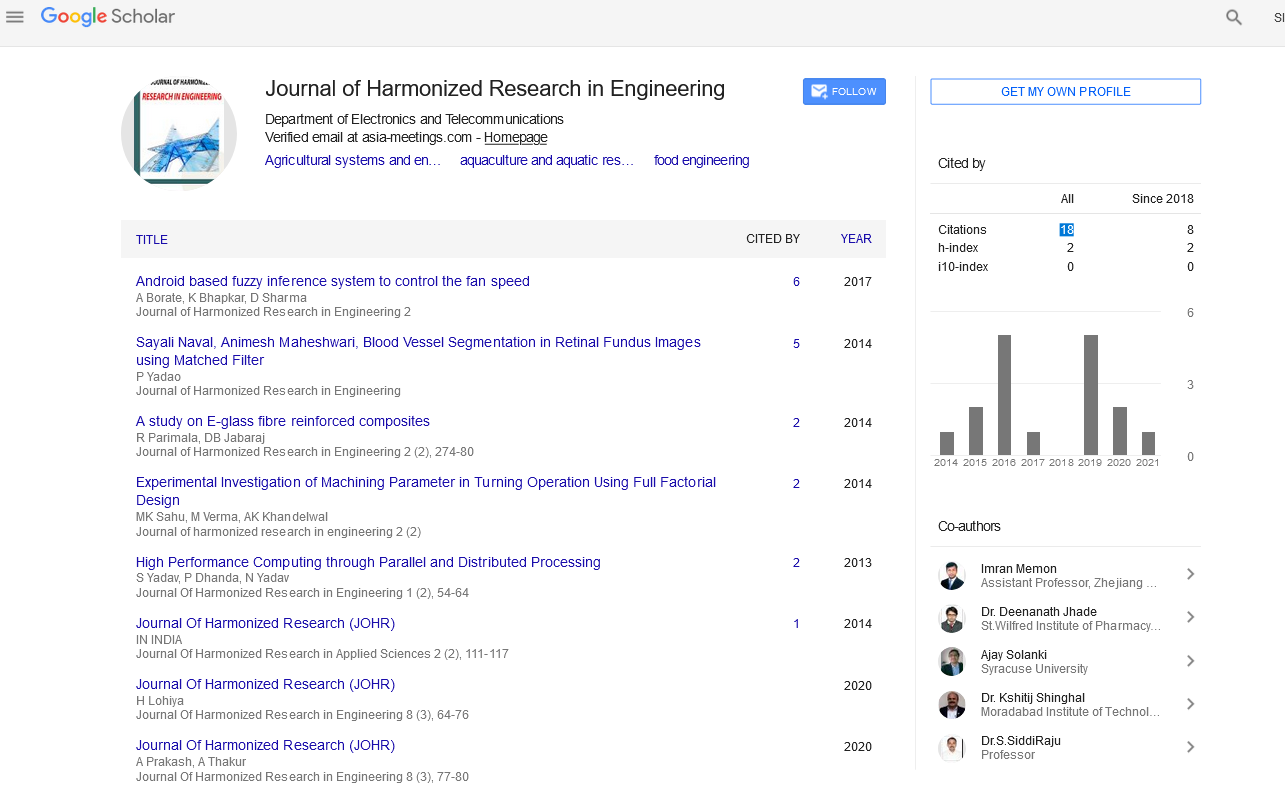
Google Scholar citation report
Citations : 43
Journal of Harmonized Research in Engineering received 43 citations as per google scholar report