Opinion Article - (2022) Volume 11, Issue 1
FACTORS AFFECTING ON THE STUDY OF DRUG-DRUG INTERACTION (DDI)
Sarvesh Sabarathinam*Received: Mar 01, 2022, Manuscript No. JHRP-22-62426; Editor assigned: Mar 04, 2022, Pre QC No. JHRP-22-62426 (PQ); Reviewed: Mar 18, 2022, QC No. JHRP-22-62426; Revised: Mar 25, 2022, Manuscript No. JHRP-22-62426 (R); Published: Apr 04, 2022, DOI: 10.30876/2321-0958.22.11.180
Description
Drug interactions can occur when a patient takes multiple drugs at the same time in one or more conditions. When taken at the same time, some medications may affect the exposure of other medications, leading to unintended reactions, toxic side effects, or, in some cases, lack of clinical efficacy. These unintended reactions are called drug interactions. As the global phenomenon of polypharmacy continues to grow, it is important for drug developers to understand how the drugs interact with each other. Various types of clinical and non-clinical drug developers use to test whether DDI can occur and whether it is significant enough to justify dose adjustments, precautions, or contraindications. Extrinsic factors (drugs, foods, or alcohol) and endogenous factors can affect the Pharmacokinetic (PK) or Pharmacodynamics (PD) properties of a drug and cause drug-drug interactions. Drug interactions can occur when a patient takes multiple drugs at the same time in one or more conditions. When taken at the same time, some medications may affect the exposure of other medications, leading to unintended reactions, toxic side effects in some cases, lack of clinical efficacy, these unintended reactions are called Drug Interactions (DDIs).
Factors that affect the PK or PD of a drug can cause drug interactions. Drug-drug interactions are primarily associated with the effects of endogenous or extrinsic factors on PK. However, in some cases, there are factors that affect the PD of the drug. The presence of food at the absorption site in the gastrointestinal tract can accelerate or interfere with the absorption process and increase, decrease, or delay concentration levels. Drug alcohol can interact with many drugs that act on the central nervous system, most commonly exacerbating the side effects of central nervous system depression. The condition can cause serious physiological changes that can alter the PK or PD of the drug, it can interfere with testing in the laboratory by causing false positive or false negative results. DDI classifications can provide important insights on how to predict, recognize, and avoid unwanted interactions. There are many considerations as to which nonclinical and clinical interaction studies should be conducted. Protocol development depends on several factors, including, but not limited to, medication planning, exposure-related safety concerns, and DDI mechanisms. DDI research can be performed at any stage of drug development, but the sooner a program can perform DDI research, the better. The results of nonclinical DDI studies combined with clinical PK data can often be used to simulate several clinical DDI studies through modeling.
In silico modeling can be performed at almost every stage of drug development, but nonclinical studies usually give the most useful results. Once the data are available, clinical DDI studies can be used to validate the DDI model. Other useful data sources include in vitro or in vivo data for parameterizing the degree of interaction between the drug and the enzyme or transporter associated with it. Individual characteristics can affect whether drug interactions occur and whether they are harmful. Details about the drug, such as dosage, prescription, and dosage, can also make a difference. A drug prescription is a specific mixture of ingredients contained in a drug. Prescribing a medicine is important because it can partially determine how the medicine works and how effective it is in the body.

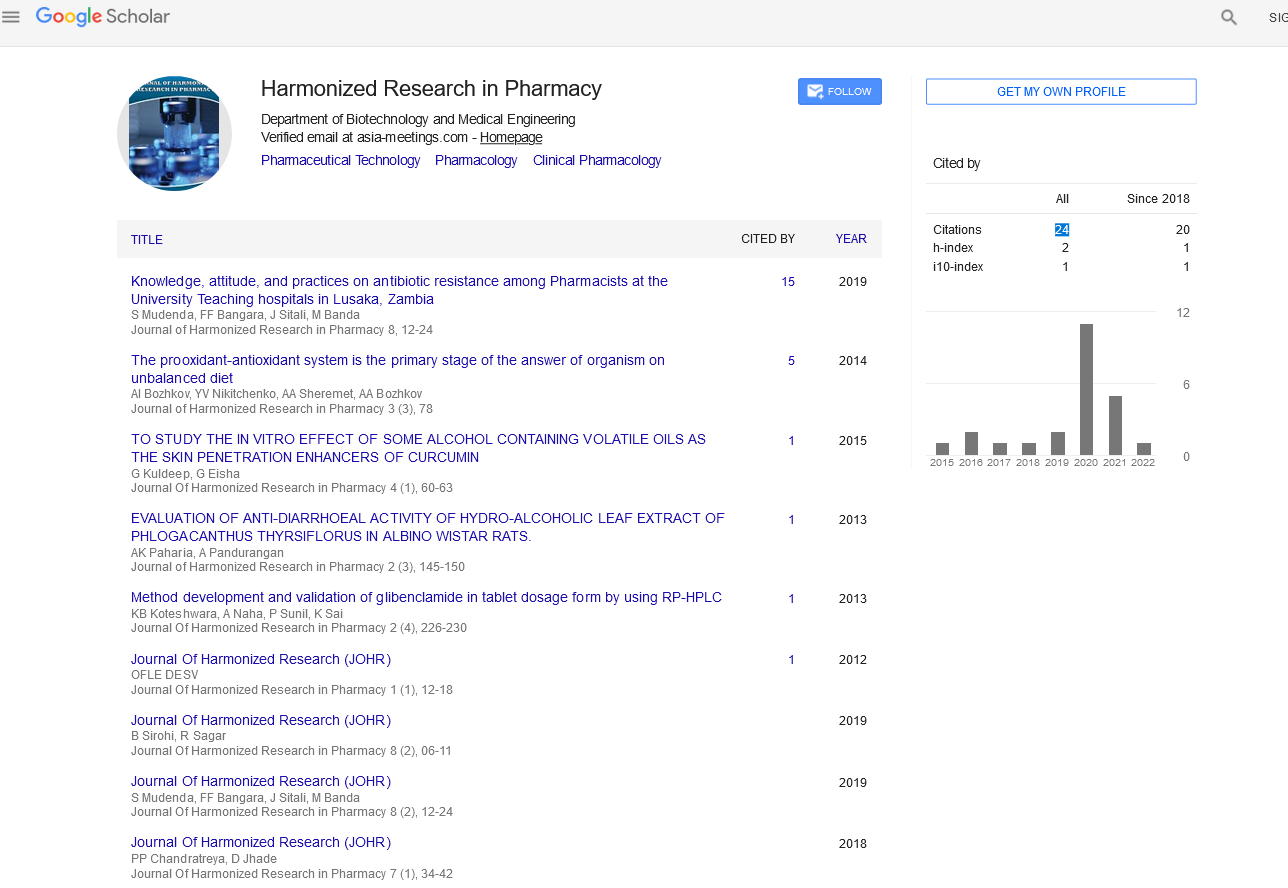
Google Scholar citation report
Citations : 147
Journal of Harmonized Research in Pharmacy received 147 citations as per google scholar report