Commentary - (2022) Volume 8, Issue 1
MANAGEMENT AND LEADERSHIP COMPETENCE FOR HOSPITAL MANAGERS
Yukio Mishima*Received: Mar 02, 2022, Manuscript No. JHRP-22-63002 ; Editor assigned: Mar 07, 2022, Pre QC No. JHRP-22-63002 (PQ); Reviewed: Mar 21, 2022, QC No. JHRP-22-63002 ; Revised: Mar 28, 2022, Manuscript No. JHRP-22-63002 (R); Published: Apr 07, 2022, DOI: 10. 30876/2454-5384.22.8.123
Description
Few studies have been conducted in the last 15 years to understand the competence requirements of healthcare managers. This is a new field of study where health care competencies have emerged, with competency-based education and training concepts primarily in the United States, United Kingdom, Australia, and some European countries. These global competencies can be validated and used in countries that have not yet developed their own management competency framework to guide workforce training and capacity building in medical service management. However, note that management capacity varies from situation to situation and related behavioral elements identified in studies conducted in one health situation/country may not be 100% applicable to other health conditions/countries. For example, the behavioral aspects of each competency of Australian and Iranian hospital managers may not be equally important. In addition, the behavioral aspects of each competency may not be equally important for different leadership levels and types of leadership positions. For example, behavioral factors that are important to the hospital director may not be considered equally important to the nursing director if the primary responsibilities that the nurse must perform are different. The six core competencies contained in the MCAP framework have been agreed upon in recent studies. Therefore, there is no doubt about their importance as core competencies that healthcare providers need to acquire in order to perform administrative tasks effectively. Although the MCAP framework contained behavioral elements related to professionalism competencies, systematic literature reviews and mappings confirmed that professionalism should be included as an individual competency for medical service managers. Professionalism is defined as “the ability to align personal and organizational behavior with ethical and professional standards, including responsibility to patients and communities, direction of service, and commitment to lifelong learning and improvement.” Now a day’s medical institution, especially hospitals, are adopting a patient-centric approach. In order for patients to receive quality service, healthcare providers must adhere to high professional and ethical standards and keep up-to-date knowledge and information. The purpose is to monitor and maintain the quality and standards of management performance. Therefore, professionalism requires further development of education and training in the healthcare field. Managers can access managerial professional development through a variety of ways. There is number of useful mechanisms including formal education at universities in the field of management; in- service training; in-house use of mentors and study groups; offsite intensive training, and seminars and conferences for achieve it. To facilitate managerial development, it has been suggested that competency based education and training for health services managers be established and adopted. The proposed framework together with a specific assessment process can be used for promoting, monitoring and evaluating the competence of health service managers, guiding the design of position description, recruitment, and assessing the competency gaps, hence training needs evaluation of executives. In addition, this model serves as a benchmark for training and empowerment of managers in healthcare organizations. Recognizing the importance of competency-based training in healthcare provider development and workforce development in the short term, identifying and developing management competency frameworks is an existing informal and official conference for healthcare providers. Supporting the need for leadership in the medical industry also contributes to the effectiveness and efficiency of providing medical services. In the long run, this framework will reflect the capacity needs of the healthcare management workforce as a whole, improve the workforce’s overall capacity, and prepare the future workforce for constant challenges and changes.

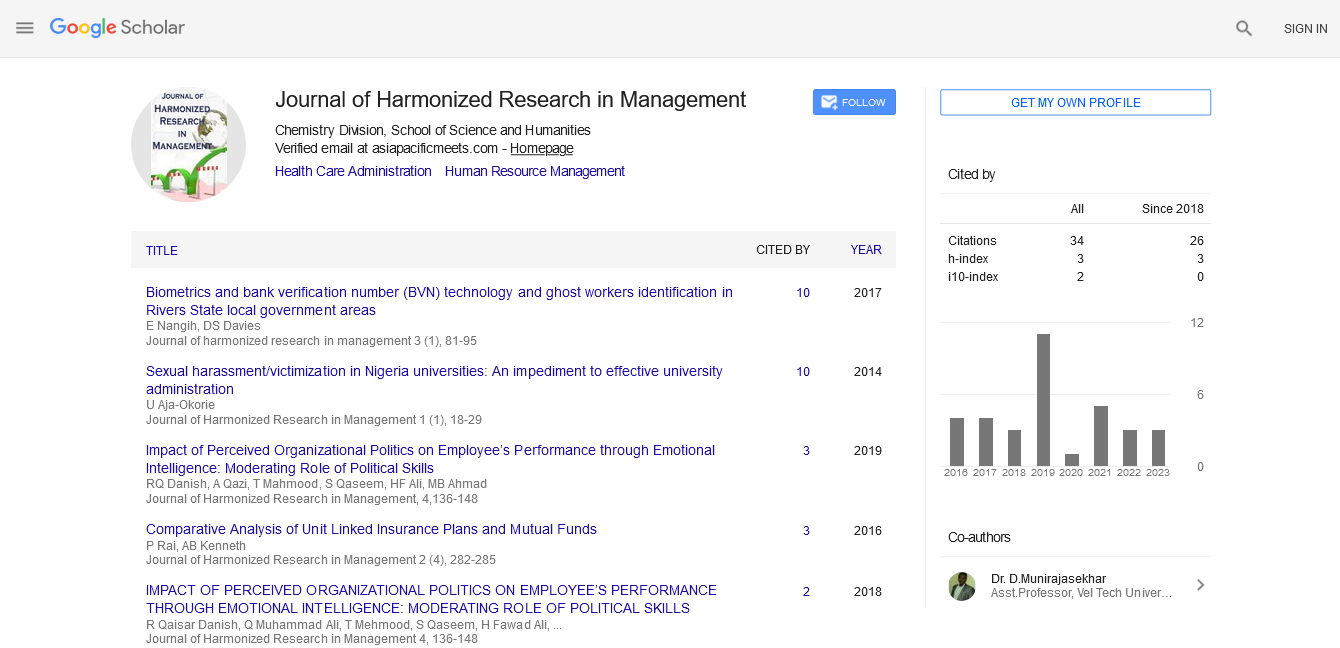
Google Scholar citation report
Citations : 92
Journal of Harmonized Research in Management received 92 citations as per google scholar report